Introduction
Multiple gestations account for 3% of live births and are rising in incidence
Twin pregnancy is the most common type of multiple gestation.
Higher order multiples are pregnancies involving three or more fetuses.
More dangerous multiples like triplets and quadruplets are therefore always delivered through C- section because the last one may be in danger should such a delivery attempt be attempted in the vagina.
Elective C-section is often performed in twin pregnancies, and it largely depends on fetal factors.
Types of Twins
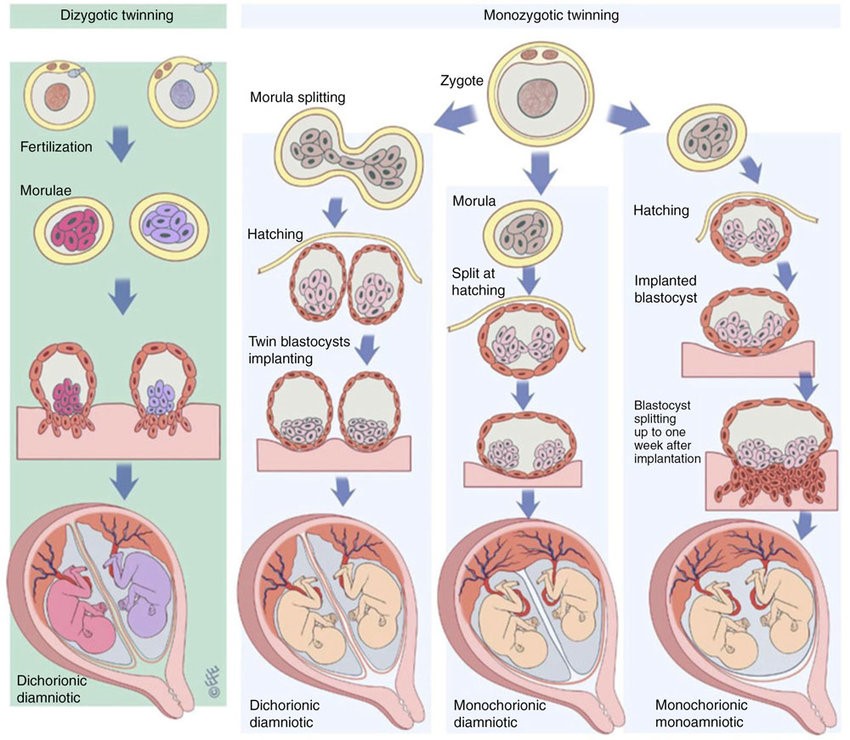
Dizygotic Twins
It is the result of fertilization of two separate ova by different sperm and simultaneously implanting and developing.
Characteristics
It is the most common form of twins (70%).
Named as non-identical or fraternal twins.
Always has two placentas (dichorionic) and two amniotic cavities (diamniotic)
Either same-sex or different-sex pairings of fetuses
Risk Factors
Growing maternal age
Family history
Increasing parity
Monozygotic Twins
- It is due to division of one already formed embryo into two embryos
- All monochorionic pregnancies are monozygotic but not all dichorionic pregnancies are dizygotic
Features
They are genetically identical; thus, they will always be the same sex. They would have shared an amniotic cavity and/or chorion if the embryo split at any stage of development.
• Division within 3 days: Dichorionic, Diamniotic (DCDA)-30%
• Division b/w 4 7 days: Monochorionic, Diamniotic (MCDA)-70%
• Division b/w 8-12 days: Monochorionic, Monoamniotic (MCMA) =<1%
• Division > 12 days: Conjoined (Siamese) twins
Risk Factors
No detectable risk factors
Constant incidence of 1 in 250.
Small rise in risk after IVF.
Not affected by race, family history, or parity.
Diagnosis
Signs & Symptoms
- Hyperemesis gravidarum (severe vomiting)
- Uterus is larger than expected for dates.
- Three or more fetal poles may be palpable.
- Two fetal hearts may be heard on auscultation.
- Maternal serum alpha-protein is excessively higher than with one fetus.
- Excessively elevated β-hCG levels.
Chorionicity
Key findings on ultrasound that helps determine the Chorionicity are:
Dichorionic
- Fetuses of different sex.
- Thick inter-twin separating membrane.
- Tongue of placental tissue within base of membranes lambda sign.
Monochorionic
- Absence of lambda sign
- Thin-inter twin separating membrane.
Differential Diagnosis
- Polyhydramnios; Uterine fibroids
- Urinary retention; Ovarian masses
Fetal Complications
| Complications | Dichorionic Pregnancy | Monochorionic Pregnancy | |
| 1 | Miscarriage | Risk of late miscarriage is 2% | Risk of late miscarriage in 12% |
| 2 | Perinatal Mortality | 3.8% per 1000 births | 38% per 1000 births |
| 3 | Fetal Defects | Each fetus carries a risk for abnormalities that is similar (1%) to singleton pregnancy. Each fetus carries a risk for abnormalities that is similar (1%) to singleton pregnancy. | Each fetus carries a risk for abnormalities that is twice (2%) to singleton pregnancy, Therefore the chance of anomaly is eight times that of a singleton. |
| 4 | Preterm Delivery | Risk of preterm delivery is 15% | Risk of preterm delivery is 25% |
| 5 | Chromosomal Defects | Having different genetic make-up, risk of chromosomal abnormalities is twice as for singleton pregnancy. | Having same genetic make-up, risk of chromosomal abnormalities is same as for singleton pregnancy. |
| 6 | Unique Complications | Increased risk of cord accidents | Twin-to-Twin transfusion syndrome Anemia-Polycythemia Sequence |
| 7 | Death of one Fetus (in 2nd or 3rd trimester) | Is associated with onset of labor. However, pregnancy may continue uneventful in some case to term. | Is associated with immediate complications in the survivor (e.g. death, brain damage). Delivery of the at-risk fetus should be avoided before 30 weeks if possible. |
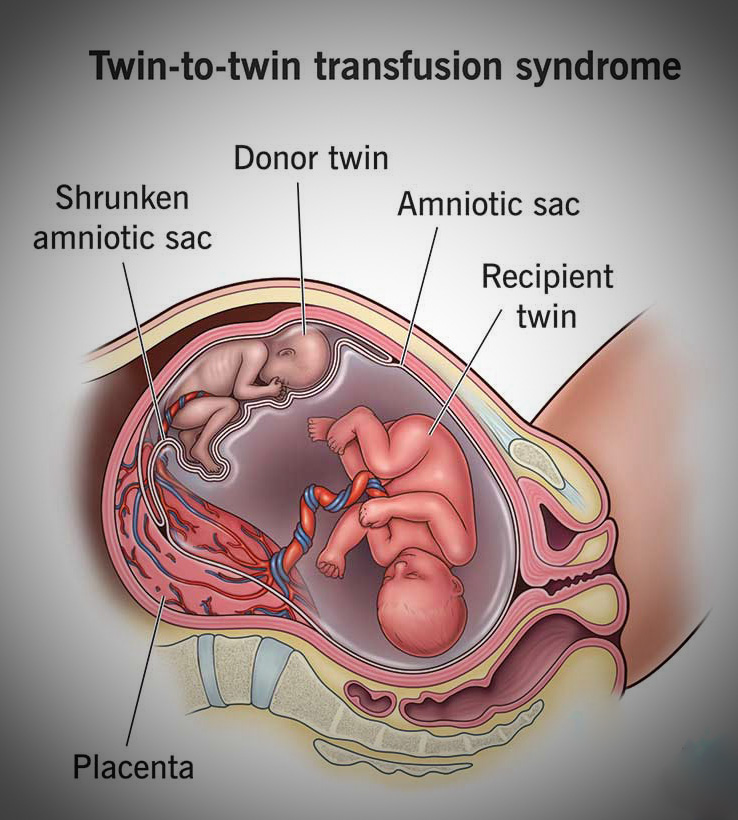
Twin-to-Twin Transfusion Syndrome (TTTS)
This is a complication that is peculiar to monochorionic twin pregnancy.
It is caused by abnormal vascular anastomoses within the placenta which distribute the fetal blood, thus causing transfusion of blood from donor twin to recipient twin.
TTTS is observed in 10% of Monochorionic Diamniotic Twins.
TTIS is observed in 5% of Monochorionic Monoamniotic Twins.
Types of Vascular Connections:
Arterio-venous (AV)
Arterio-arterial (AA)
Veno-arterial (VA)
Veno-venous (VV)
Unbalanced arteriovenous (AV) connections are responsible for TTTS. Arterio-arterial (AA) connections are protective against TTTS.
Effects on the Fetus
| Donor Twin | Recipient Twin | |
| 1 | Smaller | Larger |
| 2 | Oligohydramnios | Polyhydramnios |
| 3 | Hypovolemic and anemic | Hypervolemic and polycythemic |
| 4 | Evidence of growth restriction | Evidence of fetal hydrops |
| 5 | Neonatal outcome is GOOD | Neonatal outcome is POOR. |